Section 03: Specialty
The patient journey for specialty medications can be complex as it involves safety and educational components along with reimbursement protocols that can collectively delay time to therapy 3 to 6 weeks for some therapeutic areas.12
Learn how ePA can help
How is the Industry Defining Specialty
While there is no specific definition for what constitutes specialty, it is generally agreed that they are high-cost generic or brand-name medications (average wholesale acquisition cost of more than $670) for patients suffering from complex or rare diseases. 13, 14
Unique administration (e.g. nebulizer, injections, infusions), consistent patient monitoring through lab tests or regular checkups and time-intensive up-front processes, including enrollment documentation, benefit verification, risk evaluation and mitigation strategies (REMS) and PA further compound the complexities of specialty medications. In many cases, all of these requirements must be resolved before the patient starts therapy.
By 2020, a projected 9 out of 10 top-selling drugs by revenue will be specialty and the volume of specialty PA requests is rising.15
The Specialty Patient Journey
The specialty process is complex, consisting of multiple steps that can depend on therapeutic area, payer and specialty pharmacy. The National Council for Prescription Drug Programs (NCPDP) has worked to define a framework for the specialty patient journey that encompasses each of the major steps. Despite working well for approximately half of all specialty claims (i.e. those covered under the pharmacy benefit), ePA is not widely recognized as a solution for specialty medications. As a result, PA is often the rate-limiting step of the specialty process.*
* Order of processes may vary depending on the specialty pharmacy and process flow.
† Depending on if the claim is filed under the pharmacy benefit or medical benefit, ePA may or may not be available, respectively.
Current Process
The specialty patient journey currently relies on hub services to manually fulfill steps encompassing access and reimbursement, labs and diagnostics, as well as safety and education. This low-tech process can be time-consuming and inefficient.
To simplify the specialty journey for patients and providers, the industry must strive to make manual steps an exception to a mostly electronic process.
Electronic automation is no easy task as the complete process list for a given specialty drug can encompass over 100 distinct steps, including over 50 decision steps. When done well, an electronic solution for specialty medications will enable cross-functional coordination across all healthcare stakeholders. This will limit duplication of effort for hub services, allowing them to function quickly and efficiently.
Currently, patient enrollment is confusing for providers with each specialty medication requiring a separate web portal. An ideal electronic solution will centralize patient enrollment for all specialty medications. Forty percent of providers cite PA around specialty medications as the main pain point when prescribing the drugs, and 30-50 percent of specialty PA request denials involve administrative error.16

40% of providers cite PA as the main pain point when prescribing specialty drugs vs. communication, financial assistance and time.16
Additionally, nearly half of all specialty claims are covered under the medical benefit of health plans and suffer from an inefficient PA process, lacking many of the streamlined and automated ePA functionalities available to the remaining claims (~50 percent) covered under the pharmacy benefit.17
A streamlined workflow for specialty medication benefits all stakeholders including the pharmacy, provider, payer and most importantly, the patient. A solution that includes treatment supervision functions, tracks timeliness of medication delivery (i.e. how long it took from prescription process to the patient starting therapy) and monitors medication adherence is vital to achieving positive patient outcomes.
Awareness
According to a large ePA vendor, nearly a quarter of specialty ePA volume is initiated by primary care practices (i.e. family practice and internal medicine) not conventionally associated with specialty medications.
With more primary care providers prescribing specialty medications, ensuring they are equipped to accurately and electronically complete the more complicated specialty PA requests will reduce errors and help patients get on therapy faster.
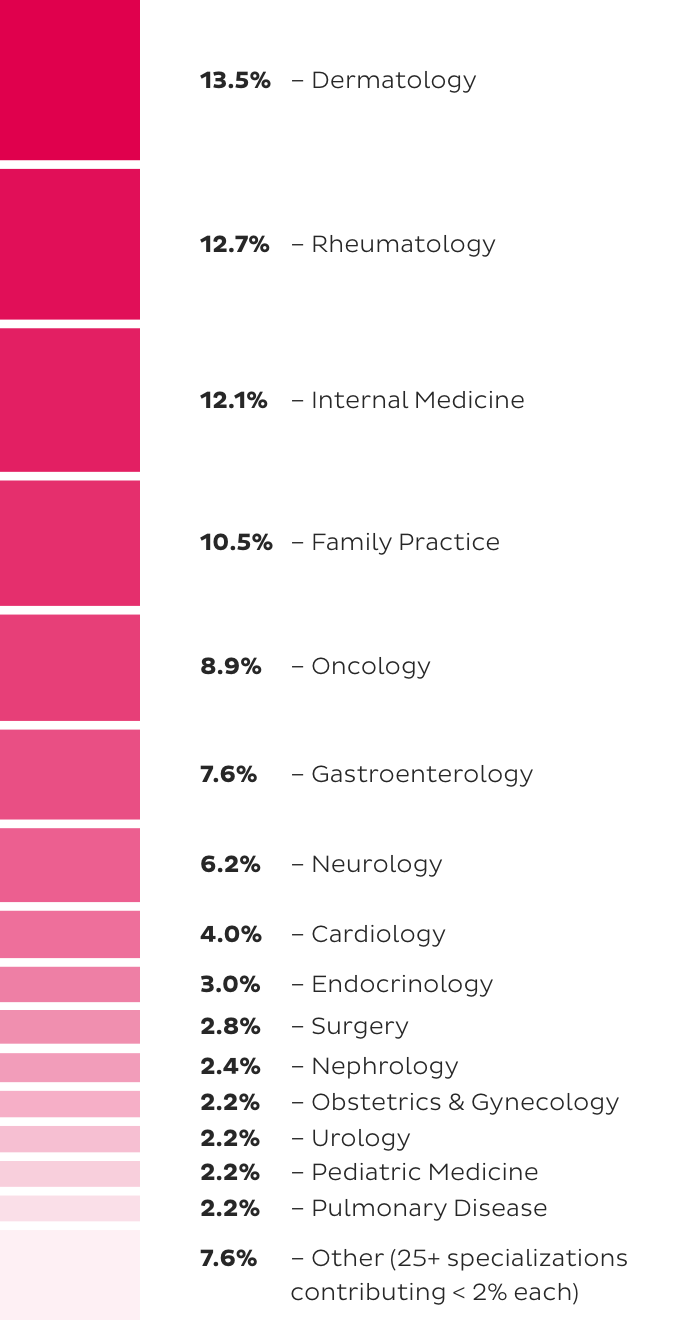
Top Specializations Starting PA Requests by Volume in 2018.
Completion Time
In today’s specialty landscape, E-Prescribing can be challenging for providers due to the complexity of determining coverage and limited pharmacy distribution.
A common question is if ePA can be used for a specialty medication, even though E-Prescribing does not offer the ideal solution. The answer is yes. In fact, ePA for specialty medications can reduce time to therapy more than tenfold (17 days to as few as 1.5 days).19
The volume of PA requests submitted electronically through a large ePA vendor has increased over 1000 percent since 2014.20 This trend is expected to continue as more providers recognize the value of ePA for specialty and more specialty drugs are prescribed (specialty drug spending is projected to reach 47 percent of pharmacy revenue by 2022).13
Key Takeaway
In 2018, over 400,000 NPIs submitted ePA requests for specialty medications,21 a 33 percent increase from last year, indicating providers are willing and eager to adopt electronic solutions that can decrease time to therapy. A PA request can be submitted through web portals, initiated at the pharmacy or through a doctor’s EHR. Unfortunately, electronic solutions do not yet account for the additional factors that prescribers care about such as enrollment forms and pharmacy visibility.
Prior authorization is one component of a very complicated process that stands to benefit from technological innovation.